Does mental illness occur before or after drug addiction?
Studies show that people who suffer from mental illness are more likely to become addicted to a substance, often called “self medicating”. Conversely, people who have suffered from addiction for years may later get diagnosed with a mental illness, this is called “dual diagnosis”. Some individuals are mentally ill to start and use drugs and/or drink alcohol to alleviate their symptoms, while others become mentally ill as a result of taking drugs or drinking alcohol.
It is important to note that according to National Institute on Drug Abuse people are most likely to begin abusing drugs including tobacco, alcohol, and illegal and prescription drugs during adolescence and young adulthood. Adolescents experiment with substances for a variety reasons including the desire for new experiences, attempts to deal with problems, and peer pressure.
Certain risk factors play a role such as genetics, coping mechanism, depression, anxiety, ADHD, bipolar disorder and schizophrenia in some one choosing addictive behaviors. Studies show that people who are diagnosed with mood or anxiety disorders are nearly twice as likely to have a substance abuse problem compared to the general public. People who suffer from anxiety find that alcohol diminished their symptoms and people who suffer from depression experience relief from taking euphoric drugs, such as marijuana, cocaine or heroin.
Some substances have been associated with the development of disorders. Rather than bringing relief due to an ongoing mental health problem, drugs can actually cause new problems to develop. According to “Substance Abuse and Mental Health Services Administration” a few of the mental health concerns that could spring to life in people who use and abuse substances are:
Deliriums- People who have this condition tend to shift between mental states with extreme speed, they may display an inability to remember detail and pay attention to the events taking place around them. They might seem angry and irritated, or depressed and apathetic, and they might struggle to keep their arms and legs still.
Psychosis- Similar to deliriums, in that people who have this particular condition also seem jittery and unreasonable. They might claim to hear voices that others cannot hear, or they might seem as though they’re looking at places and faces others can’t see. They might become angry and violent, and they might be unable to stay still and calm. People in a psychotic state can be remarkably dangerous, simply because they can’t be reasoned with.
Hallucinogen-Persisting Perceptual Disorder- Similar to psychosis, in that people who have this disorder often experience visual hallucinations, such as: streaks of color, halos of light, movement trails and/or floating objects in the field of vision.
Persisting Amnestic Disorder- This condition often accompanies the long-term use of drugs, and it can cause an inability to put down new memories or to access old memories. The portions of the brain that control these vital processes have been damaged by drugs, and the severity of the disorder can range from mild to severe, depending on the amount of damage that has been done.
Persisting Dementia- This is similar to persisting amnestic disorder in that people who have this disorder might also struggle with memory. However, these people also have difficulties involving learning and attention. The degree of impairment is dependent on the drugs the person has used.
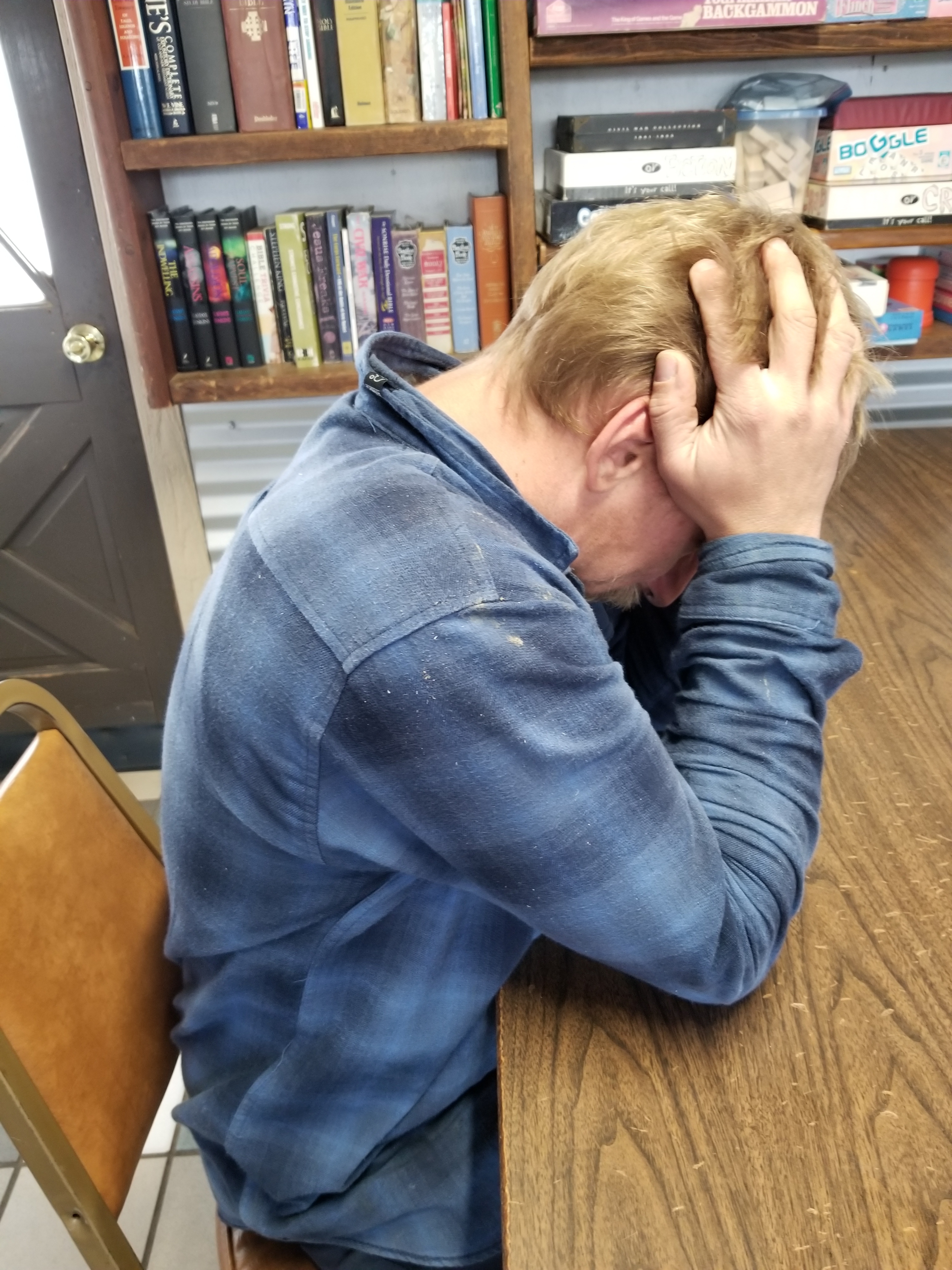
Mood Disorders- Mood disorders might not seem severe when they are placed beside dementia disorders, but people who feel relentlessly depression might face many of the same types of symptoms. They also find it hard to pay attention and learn new information and they might struggle to remember details from the past. People with this disorder might also find it hard to muster up the energy to get through the day.
Sexual Dysfunctions- Sexual dysfunctions can go alongside a mood disorder, but some people who abuse drugs also find it difficult to participate in sex at all, whether or not they feel depressed. In some cases, some people have a psychological desire for intimacy, but their bodies won’t comply. in other cases, there is no psychological desire at all.
Sleep Disorders- Sleep disorders can also take hold in people who have a history of drug abuse, and this can also take many forms. Some people find it difficult to fall asleep, as their mind stay active even when their bodies are exhausted. Others find it hard to stay asleep, as they awaken repeatedly rather than resting soundly.
Anxiety Disorders- Anxiety disorders can be similar to sleep disorders, in that they make people feel restless and ill at ease, but people with these disorders may feel this way all of the time, not just at night.
In some cases, it is difficult to know what came first-the substance abuse or the mental health disorder. It can also be difficult or impossible to determine causality; even if the symptoms of one condition appeared first, it may not have caused the other. What is known is that it is relatively common for people to self-medicate mental health symptoms with substances. Also, substance abuse may worsen or bring about symptoms of mental illness. For example Marijuana has been shown to increase the risk of psychosis for some users. The relationship between opioid abuse and depression is bi-directional, meaning suffering from one increases the risk of the other. Opioid abuse is defined as using a prescription opioid for non-medical reasons or using it longer or in greater amounts than what was prescribed by a doctor, and opioid abuse has been linked to higher rate of depression, anxiety, and bipolar disorders. In addition, it’s long been known that heavy drinking often goes hand in hand with depression, but there has been debate about which came first-the drinking or the depression. One theory is that depressed people turn to alcohol in an attempt to “self-medicate” to ease their emotional pain. However, a large study from New Zealand showed that it was probably the other way around- heavy drinking led to depression.
Every person is an individual with their own unique genetics and experiences, therefore one size fits all approach can not be beneficial in determining the cause of addiction, mental illness, or the treatment of these conditions. Each person should be evaluated and treated as an individual without jumping to conclusions as to whether the addiction caused mental illness or was a result of mental illness. If a person is determined to have an addiction problem, special care and careful approach to diagnosis of mental illness by health care professional is paramount, as the often prescribed medications for these individuals continue the addiction and mental illness process.
Early education is a key strategy to prevent people from self medicating a mental illness with substance abuse or creating an addiction onset mental illness.
It would be prudent for every individual to recognize the dangers of addiction at an early age and refrain from using substances that can potentially develop into abuse. Even though one may feel momentary relief from anxiety, depression or any other mental issues by engaging in such behaviors, it comes with a great risk of developing an addiction and additional mental problems. Instead, if you are feeling anxious, depressed, or have other mental issues seek out healthy alternatives such as exercise, meditation and counseling to assist you. Only resort to prescription medications, if absolutely necessary, prescribed by a qualified medical professional.
~Teri Storm