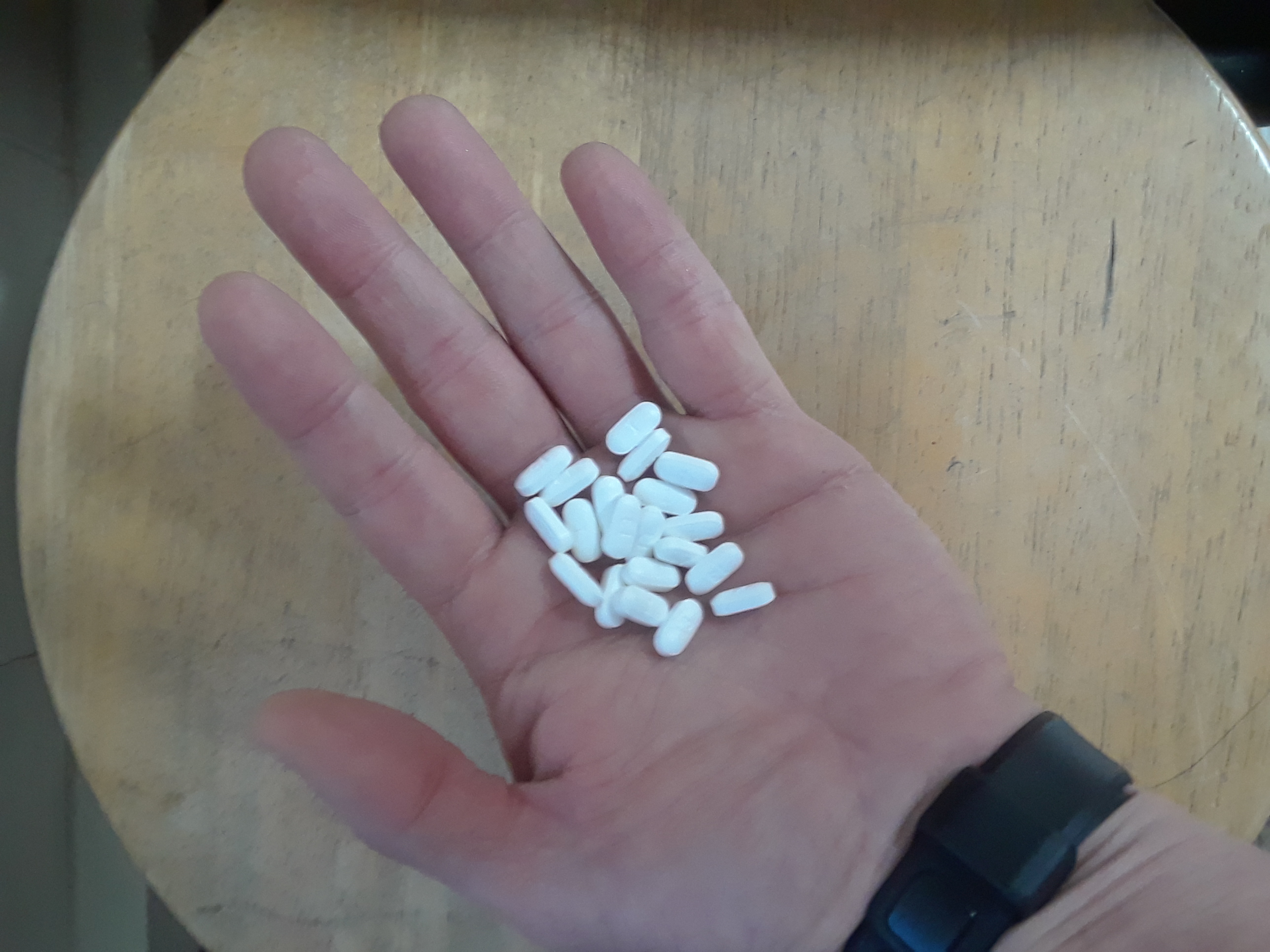
Tramadol, is a synthetic opioid pain medication used to treat moderate to moderately severe pain. It is sold under the brand name Ultram, Conzip, and Rbix ODT. When taken by mouth in an immediate release formulation, the onset of pain relief usually begins within an hour. It is also available by injection. It may also be sold in combination with paracetamol (acetaminophen) as longer acting formulations such as Ultracet. There is also an extended release version called Ultram ER.
Tramadol had its beginnings in 1977 under the name “Tramal” by a West German pharmaceutical company. In 1995 it was approved in the United Kingdom and the United States. In approving Tramadol, the US Food and Drug Administration (FDA)decision was based largely on research in which the drug was injected. The FDA also weighed evidence from Europe, where the drug had been on the market for years.
The FDA originally approved tramadol for use in 1995, and recommended it not be classified as a controlled substance. Tramadol was originally considered to have a much better safety profile than other opioid analgesics like morphine or hydrocodone and thought to have low potential for dependency and not likely to be abused. Therefore, tramadol seemed to be a better alternative than other opioids like Vicoden (Norco), Percocet or not be as dangerous as high potency medications such as morphine, Dilaudid or Fentanyl. This new drug relieved pain just as well as a narcotic like Oxycontin, but isn’t addictive. At least that is what the clinical trial showed. Therefore, tramadol was widely prescribed by doctors as a “safer” alternative to narcotics for pain.
Fast forward- Opioid abuse is epidemic in the US. From 2000-2016 the death rate for synthetic opioids except for methadone, including fentanyl and tramadol, has increased more than 20-fold, more than any other subgroup of opioids. The US Substance Abuse and Mental Health Services Administration (SAMHSA) reported that from 2005-2011 Emergency Department visits for tramadol-related misuse or abuse increased 250% from 6,255-21,649 in this six year period. Visits by males increased from 2,333 to 9,411 and visits by females increased from 3,922 to 12,238. This higher rate of ER visits in females compared to males, is the reverse from the overall higher death rate for males from all opioids combined. The greatest increase in ER visits for tramadol-related misuse or abuse was 481% in patients aged 55 and older, most likely consistent with the number of prescriptions in this age group. This research shows that tramadol has greater potential to be abused and to cause overdoses than was believed when it first appeared on the U.S. market in 1995.
What could have gone wrong in the clinical studies showing otherwise? Data from Germany had suggested it was only about one -tenth as potent as morphine when injected. Other data showed that years of use in Germany and other countries there was very little abuse of the drug. However, in the early 1990’s, researchers at Johns Hopkins University did a study in which high doses of the drug were given orally to opioid abusers. Taken orally, tramadol acted much differently than when injected. Taken by mouth, the drug is transformed in the liver to a metabolite known as M1, which is able to attach to and activate opioid receptors in the brain. It is that substance that is believed to produce the desirable, opiate-like effect similar to oxycodone , the narcotic OxyContin, one of the most abused drugs in America. In 1994, Ortho-McNeil, part of the P.W. Johnson Pharmaceutical Research Institute of Johnson & Johnson, sought approval from the FDA to sell Ultram, its brand name version of the drug in the U.S. The Johns Hopkins study was never published, but was provided to the FDA when it was reviewing the approval for tramadol. A journal Sentinel/MedPage Today investigation found that the FDA failed to heed this key piece of research indicating tramadol had the potential to be abused. Instead, the agency recommended not putting tramadol under the Controlled Substance Act. The Controlled Substance Act places drugs into five progressively restrictive categories based on their abuse potential. At the top of the list are drugs such as heroin. At the other, are some cough medicines with limited amounts of codeine. The FDA did ask Otho-McNeil, to fund a committee of paid consultants who were to watch for abuse problems that might require making it a controlled substance. That never happened. Instead, Journal Sentinel/MedPage Today investigators have showed that opioid companies paid millions of dollars to doctors and nonprofit medical societies that pushed for more liberal use of the drugs in treating chronic, noncancerous pain. Yet rigorous studies never have shown that the drugs are safe and effective when used that way. In 2013, 45 million prescriptions for tramadol were written for patients, nearly doubling in just 5 years. Due to mounting evidence of abuse among the general public, as well as evidence of withdrawal symptoms upon cessation, the Drug Enforcement Administration published revised rules in 2014 making tramadol a federally controlled drug. For 19 years many people were misled in trusting and thinking tramadol was safe. Many suffered at the expense of greedy pharmaceutical companies and doctors. Physicians should exercise extreme caution when prescribing this drug, especially to those who have a history of drug abuse.
Tramadol contains the following warnings:
-May increase risk of having a seizure
-People who are suicidal or prone to addiction should not take tramadol
-Risk for Serotonin Syndrome if combined with other serotonin raising drugs, especially
antidepressants. (Symptoms include agitation, fever, nausea, muscle stiffness, lack of
coordination and/or consciousness)
-Life threatening respiratory depression
-May be habit forming